Lyme disease is an infection caused by the bacterium Borrelia burgdorferi. Lyme disease is named after Lyme, Connecticut, where the disease was first discovered in 1975. The disease was initially called Lyme arthritis due to the unusually high numbers of patients who presented with joint complaints in those days. Later on, the black legged tick also known as the ixodes scapularis was linked to the transmission of the disease.
In the early 1980’s Dr. Borgdorfer discovered the bacterium responsible for the infection and named it borrelia burgdorferi.
This bacterium is a spirochete and related to syphilis. Syphilis is called the great imitator in medicine due to the fact that it produces signs and symptoms that mimic numerous diseases. Lyme disease is a more masterful imitator than syphilis. Lyme disease is associated with hundreds of diagnoses.

Lyme tick
In the early days of Lyme research, it was discovered that most of the affected patients lived near wooded areas that where ticks were prevalent. The patients’ symptoms usually started in the summer months when ticks were most active. Many of the early patients reported

having a peculiar skin rash. The appearance of this rash preceded the arthritic and other symptoms..
It should be noted that patients who have chronic Lyme disease usually do not remember ever having a rash or experiencing any tick bites.
How Is Lyme Disease Transmitted?
Lyme disease is most commonly transmitted through the bite of infected ticks, though the bacterium can also be spread by other insects such as mosquitoes, spiders, fleas and mites and migratory birds. Other animals such as the white-footed mice, deer, raccoons, opossums, chipmunks, foxes, shrew moles and squirrels and even horses can transmit the bacterium.
Because of the many different vectors of this bacterium, Lyme disease is present in most states of the United States.
Symptoms of Lyme Disease
In the early stages of Lyme disease, the person may experience flu-like symptoms that can include a stiff neck, chills, fever, swollen lymph nodes, headaches, fatigue, muscle aches, and joint pain. You also may experience a large, expanding skin rash known as erythema migrans (EM) around the area of the tick bite. If untreated, the infection can spread to joints (especially in the knees), the heart and the nervous system.
Erythema chronicum migrans. Erythema chronicum migrans or Erythema migrans (EM) is the telltale rash that occurs in about 70% to 80% of cases of Lyme disease. This rash starts as a small red spot that expands over a period of days or weeks, forming a circular, triangular, or oval-shaped rash. Sometimes the rash resembles a bull’s-eye because it appears as a red ring surrounding a central clear area. The rash, which can be of different sizes: It can be small or it can occupy the entire width of the arm or back It usually appears between three days and a few weeks of a tick bite, usually occurring at the site of a bite. As infection spreads, several rashes can appear with different shapes and sizes in different parts of the body. Sometimes rashes can appear and disappear years after the exposure.




Lyme Disease rashes
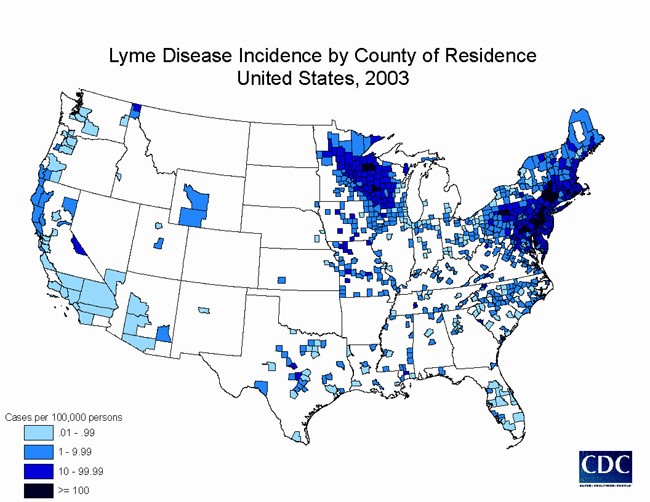
Prevalence of Lyme Disease in the USA
Erythema chronicum migrans are often accompanied by symptoms such as fever, headache, stiff neck, body aches, and fatigue. These flu-like symptoms may resemble those of common viral infections and usually resolve within days or a few weeks.
Lyme Arthritis. After several weeks of being infected with Lyme disease, approximately 60% of those people not treated with antibiotics develop recurrent attacks of painful and swollen joints that last a few days to a few months. The arthritis can shift from one joint to another; the knee is most commonly affected and usually one or a few joints are affected at any given time. About 10% to 20% of untreated patients will go on to develop lasting arthritis. The knuckle joints of the hands are only very rarely affected.
Neurological symptoms. Lyme disease can also affect the nervous system, causing symptoms such as stiff neck and severe headache (meningitis), temporary paralysis of facial muscles (Bell’s palsy), numbness, pain or weakness in the limbs, or poor coordination. More subtle changes such as memory loss, difficulty with concentration, and a change in mood or sleeping habits have also been associated with Lyme disease. Other associated neurological problems include movement disorders, chronic fatigue syndrome, and fibromyalgia.
Nervous system abnormalities usually develop several weeks, months, or even years following an untreated infection. These symptoms often last for weeks, months, or years and can be difficult to eradicate
Heart or Cardiac problems. A few people infected with Lyme disease would develop some type of heart complication from it. This could range from irregular heartbeat or, slow heartbeat (bradycardia), to orthostatic hypotension. There can also be dizziness and shortness of breath. These symptoms can be temporary or they can be chronic, especially in patients that have chronic Lyme disease.
Other symptoms. Less commonly, Lyme disease can result in eye inflammation and severe fatigue, although none of these problems is likely to appear without other Lyme disease symptoms being present.
Lyme disease imitates a variety of illnesses and its severity can vary from person to person. If you have been bitten by a tick and live in an area known to have Lyme disease, see your doctor right away so that a proper diagnosis can be made and treatment started.
Prevention
Methods include using insect repellant, removing ticks promptly, applying pesticides and reducing tick habitat.
The best way to prevent Lyme disease is to avoid wooded, bushy areas where ticks may be present. If bitten by a tick, remove the tick promptly and properly by gently grasping the tick near its head or mouth. Avoid squeezing or crushing the tick. Pull it carefully and steadily. Once the tick is removed, treat the area with an antiseptic solution.
Other methods of prevention include dressing properly if going into wooded or grassy areas. Wear clothing to cover your entire skin surface except the face. Wear hats gloves and socks to reduce tick exposure
The Great(er) Imitator
Lyme disease is called the great imitator. Another spirochetal infection, syphilis was called the great imitator by doctors decades ago because the disease had several phases which could mimic many other diseases. Lyme disease is a more artful imitator than syphilis. This disease can appear to be many other diseases like Parkinson’s disease, ALS (Lou Gehrig’s disease); Fibromyalgia; Chronic Fatigue syndrome and so forth.
The patients may appear healthy outwardly but their internal physiology is unhealthy. The organism that causes Lyme disease (B. burgdorferi) is a spirochete and is related to the spirochete bacterium that causes syphilis. They are very similar microscopically and are both capable of taking different forms in the body depending on what conditions they need to accommodate. B. burgdorferi’s corkscrew-shaped form allows it to burrow and hide in a variety of the body’s tissues, thus causing wide-ranging multi-system effects. There are currently over 100 strains of B. burgdorferi in the U.S. alone and 300 worldwide, many of which have developed resistance to various antibiotics.
Lyme disease Testing
The easiest way for a doctor to diagnose Lyme disease is to see the unique bull’s-eye rash. If there is no visible rash (as is the case in about one-fourth of those infected), the doctor might order a blood test three to four weeks after the onset of the suspected infection to look for antibodies against the bacteria. The variable signs and symptoms of Lyme disease are nonspecific and often are found in other conditions, making diagnosis difficult. In addition, ticks that transmit Lyme disease also can in some cases spread other diseases at the same time. The test used most often to detect Lyme disease is an enzyme-linked immunosorbent assay (ELISA) test. ELISA detects antibodies to B. burgdorferi but because it can sometimes provide false-positive results, it’s not used as the sole basis for diagnosis. This test may not be positive during the early stage of Lyme disease, but the rash is distinctive enough to make the diagnosis without further testing in people who live in areas infested with ticks that transmit Lyme disease. If the ELISA test is positive, another test — the Western blot — is usually done to confirm the diagnosis.
Western blot. This is a two-step test. This test detects antibodies to several proteins of B. burgdorferi. A polymerase chain reaction (PCR) test helps detect bacterial DNA in fluid drawn from an infected joint. It’s not as effective at detecting infection of blood or urine. It’s used for people who may have chronic Lyme arthritis. It may also be used to detect persistent infection in the cerebrospinal fluid of people who have nervous system symptoms. The test is ordered when the ELISA result is either positive or uncertain.
It should be noted that in the first few weeks following exposure to the organism, antibody tests are not reliable because the patient’s immune system would not have produced enough antibodies to be detected.
Other tests. At our practice, we often use one of the local and or national laboratories to test for Lyme disease. In addition to Lyme, we also test for co-infections like Cytomegalovirus (CMV); Babesia; Ehrlichiosis; Chlamydia pneumoniae; Epstein-Barr virus (EBV); Human Herpes Virus 6 (HHV-6); Mycoplasma; Bartonela and Candida. We also test for food allergies and heavy metal analysis in our workup.
Making the correct diagnosis is crucial in this disease and this greatly impacts the correct treatment plan. This is why we recommend certain laboratories for these specialized testing.
Treatment
At GMA, our Lyme patients have chronic Lyme disease. These are patients who were diagnosed with Lyme many years after contracting the bacterium or who present to us with a panoply of symptoms and after appropriate examination, history and laboratory studies, are diagnosed with Lyme disease. These patients would present with a whole host of symptoms including fibromyalgia, malaise, chronic fatigue, memory impairment (brain fog and frank memory loss and cognitive problems), and so forth. Our approach to treatment is a very comprehensive approach. We believe and research has shown that long-term antibiotic therapy, while beneficial to some extent, cannot totally eradicate Lyme.
GMA approach to Lyme disease
Acute Lyme disease is easy to treat. By acute we mean that someone is infected with the Lyme bacterium and he or she presents to a healthcare professional within three months of the infection. In all likelihood, that patient could be cured of Lyme disease with three to four weeks of oral antibiotics.
On the other hand, when a patient has chronic Lyme disease (that is an infection that has been present for six months or longer) and in some cases that we see, several years, and the patient’s symptoms have gone unrecognized as Lyme disease, it is difficult to treat and eradication or total suppression of the infection would require a very comprehensive approach. Antibiotics are not the cure; even high-dose, long-term intravenous antibiotics cannot eradicate or totally suppress chronic Lyme disease. Because chronic Lyme disease is a complicated infection that affects many body systems, it is truly a disease complex. Therefore, its treatment must employ a comprehensive approach. At Grace Medical, we use an advanced integrative approach to treating this complex disease. What we have found to be the most effective approach is the following protocol consisting of:
1. Whole body detoxification. Here, we use EDTA chelation therapy to detoxify the body and reduce free radical load, especially where heavy metals are present in the body.
2. Dietary Counseling. Avoid diets that produce high free radical load. We would advise our patients to reduce diets that produce high levels of inflammation. For example, processed foods and simple carbohydrates are highly inflammatory foods.
3. Behavioral modification. Here we advise our patients on proper sleep habits and stress reduction.
4. Oxidative therapies. This would include Ozone therapy; Hydrogen peroxide infusions and
high dose Vitamin C infusions. We also employ Ultraviolet Blood Irradiation or UBI.
5. Hormone testing and balancing. This could include thyroid hormone replacement as well as other hormones.
6. Potent supplements to boost energy and improve sleep as well as proper gastrointestinal functioning.
7. Phospholipid exchange therapy. Every mammalian cell has phospholipids in its cell wall. Therefore, these molecules are extremely important in the way the cells function; and in information transmission in and out of the cell.
8. Nutrient Infusions. These could be modified to Myer’s cocktails which are beneficial in increasing the energy level of the patient.
Lyme Controversy
Lyme disease has become very controversial all across the country. This ought not to be so. Lyme disease is a REAL disease. More than 300 diseases and conditions are associated with Lyme disease complex. Estimates are that there are anywhere from 30,000 up to 300,000 new cases every year in the United States. This is a major public health concern. The majority of patients are misdiagnosed (underdiagnosed) and given other diagnoses. The Lyme disease organism exists in the body in different forms at the same time. These include the adult organism, cystic forms and forms hiding in Biofilm. Lyme disease is a clinical diagnosis, therefore, the absence of antibodies does not rule out the disease. There are many stumbling blocks that patients with this disease complex face. First, the proper testing must be done using a Lyme-competent laboratory. Co-infections and other disruptions of the body must be sought, eg. Heavy metals; food allergies, etc. Secondly, the correct interpretation of the test results must be done. We often see chronic Lyme disease labeled and treated as acute Lyme disease. And thirdly, the treatment plan must be comprehensive and properly targeted so as to obtain the best outcome and the restoration of the patient’s health.
At Grace Medical, we have decades of experience treating Lyme disease and we are very Lyme Literate. If we can help you, do not hesitate to contact us.

